Illustrations by Eva Giurco
What should I expect after the treatment?
After any treatment, the patient will start a regular check-up program. The purpose of these checks is to verify your health’s state and the tumor localization site; during the visits the patients has the opportunity to ask questions and receive clarifications. So, during each control visit:
- The patient will be visited
- He can ask questions and receive clarifications
- Specific radiological examinations may be required
Can Desmoid Fibromatosis come back?
Desmoid Fibromatosis can return after the first-line treatment; in this case we speak about recurrence. In other cases, DF can remain stable for several years and then begin to grow. If you have a recurrence or the tumor should start to grow again, your Doctor will propose the most suitable treatment strategy, in agreement with the multidisciplinary team.
Follow up
Due to its unpredictable nature, Desmoid Fibromatosis is followed through regular radiological examinations.
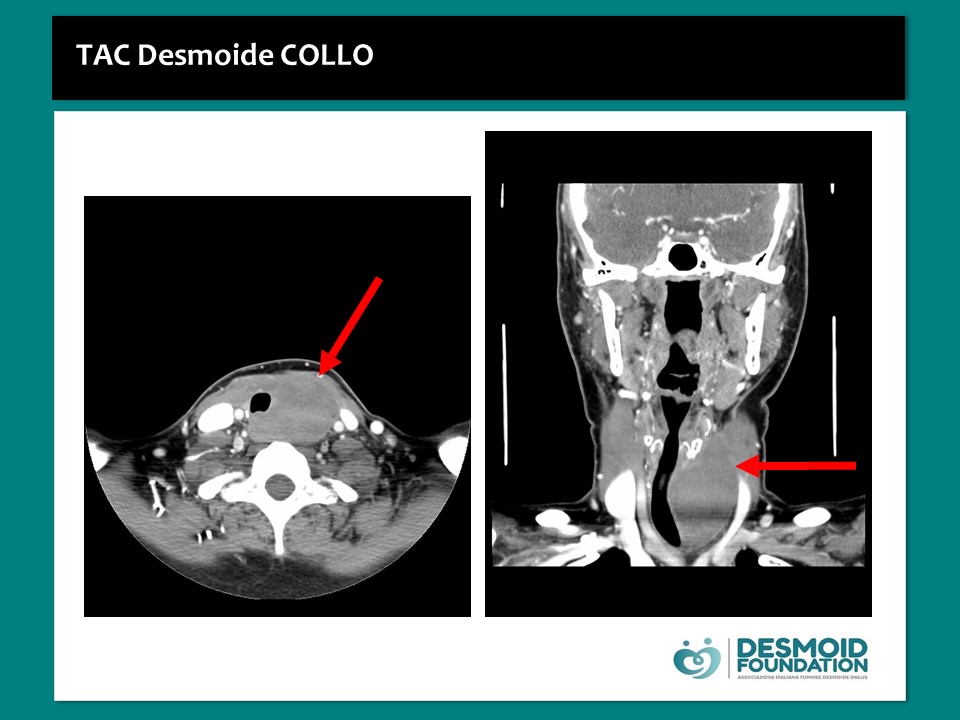
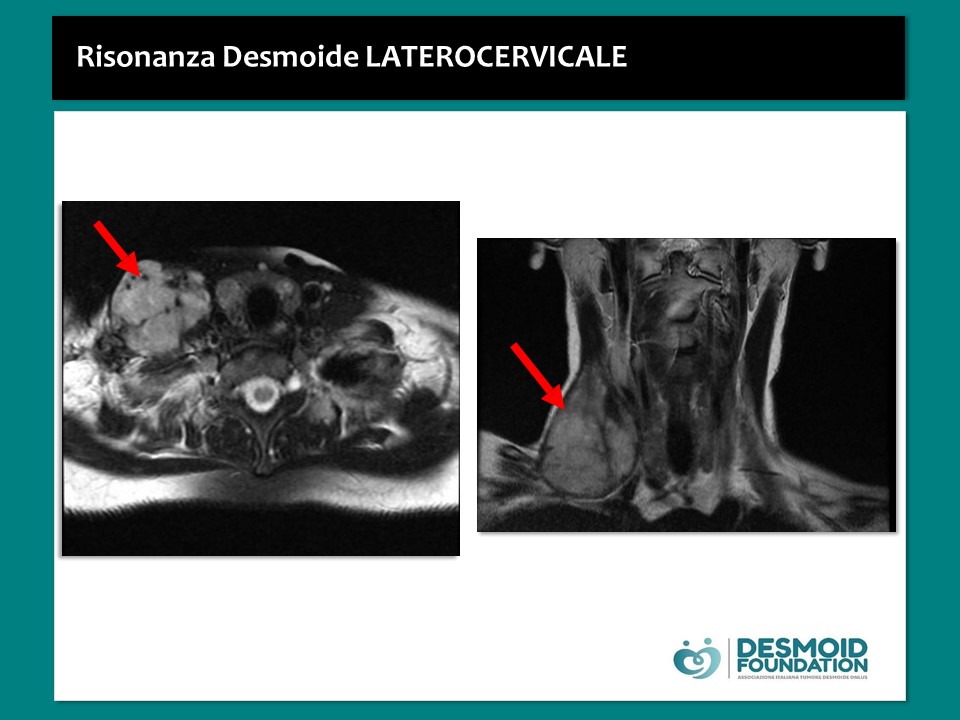
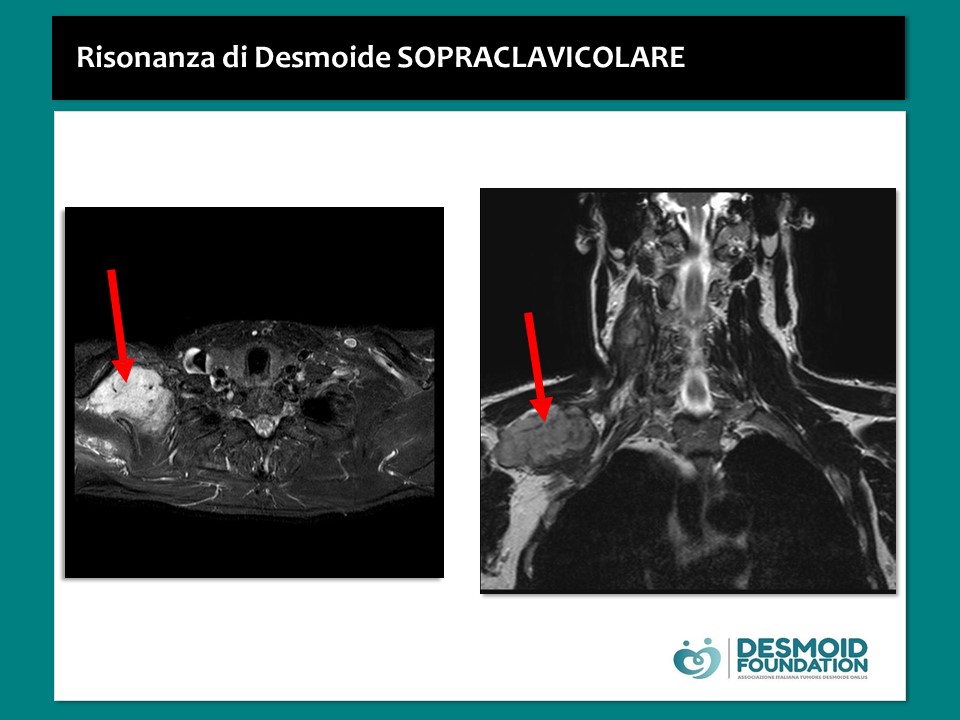
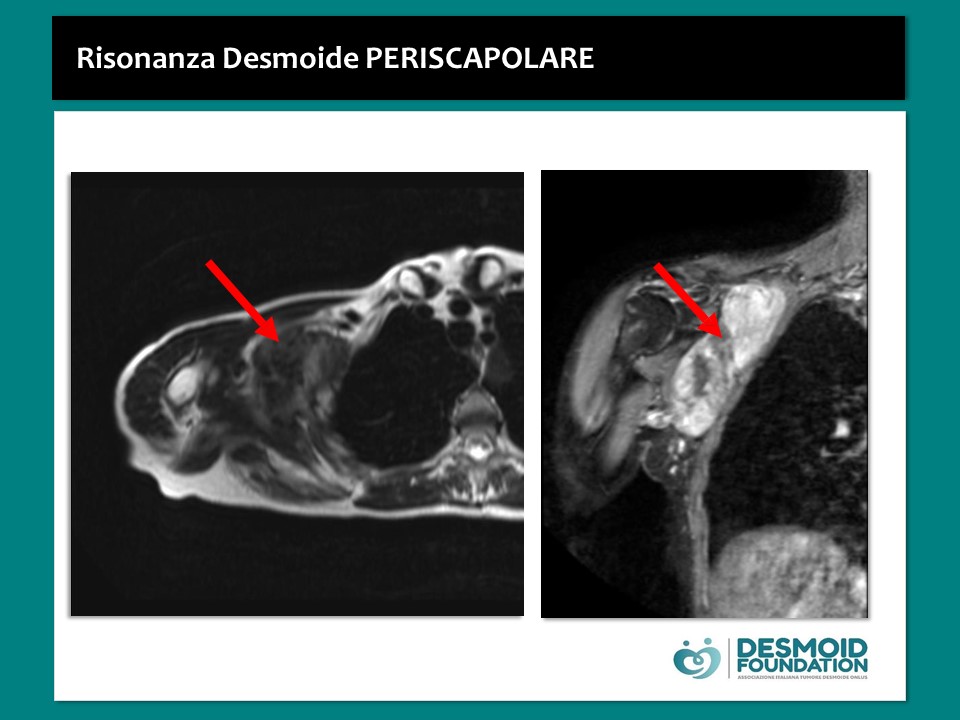
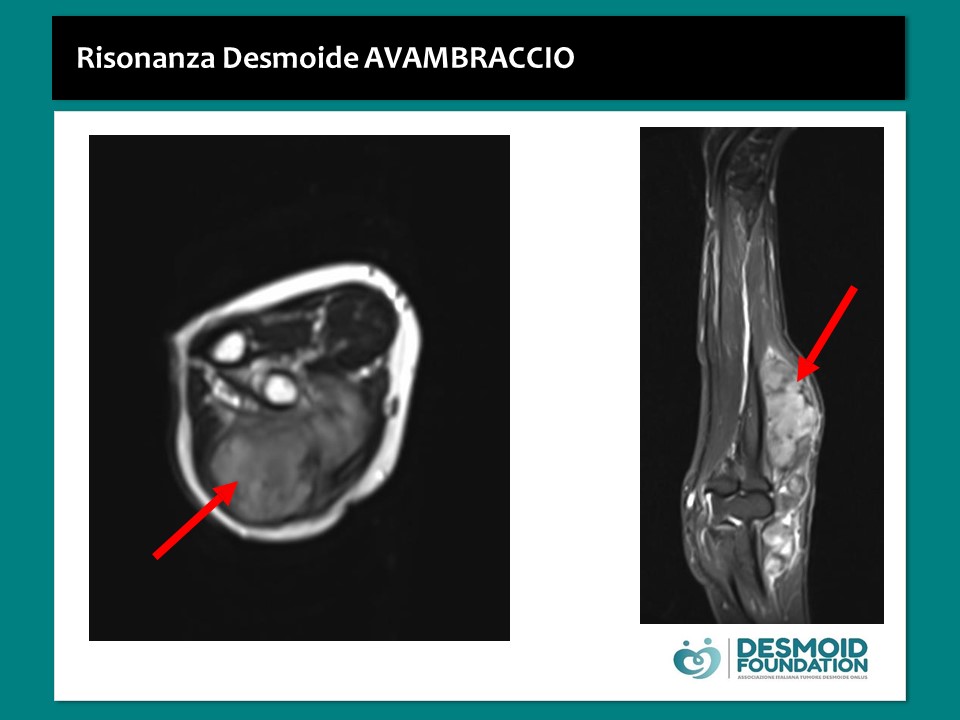
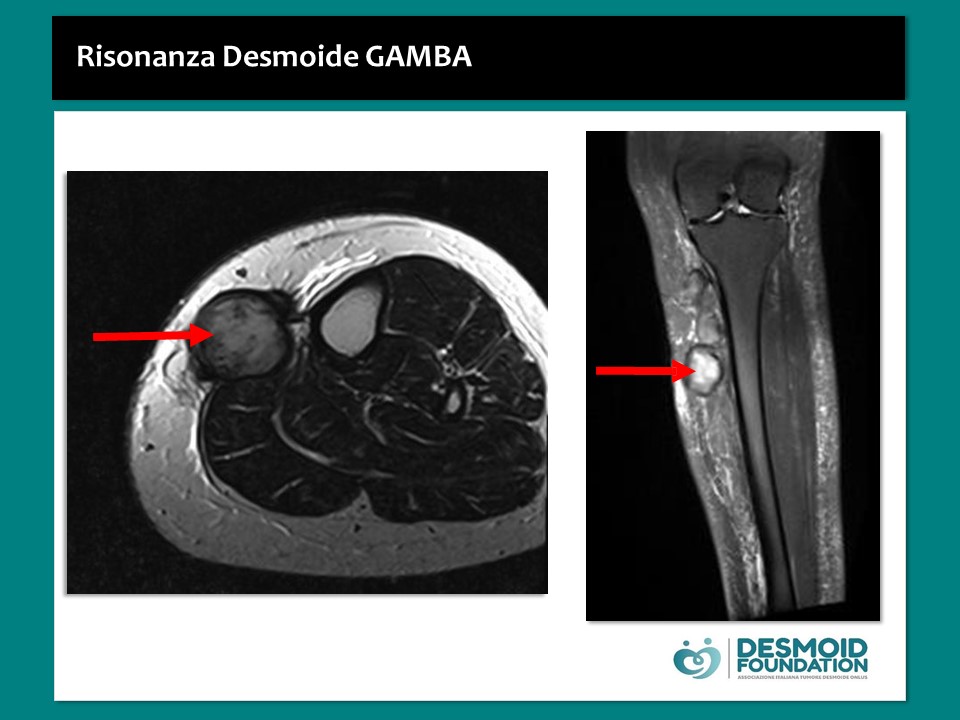
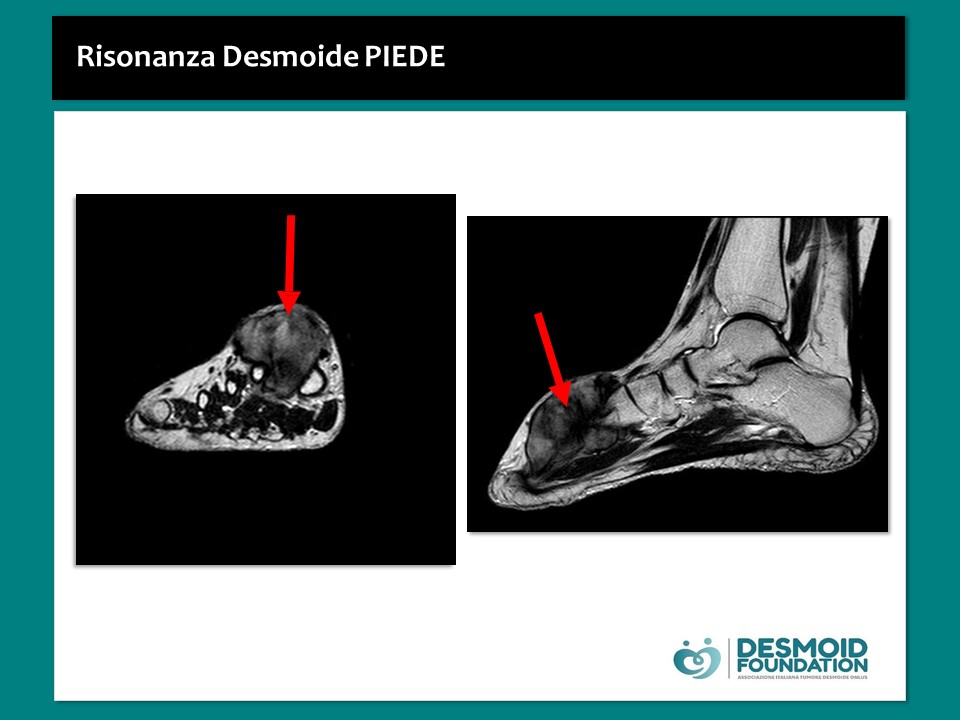
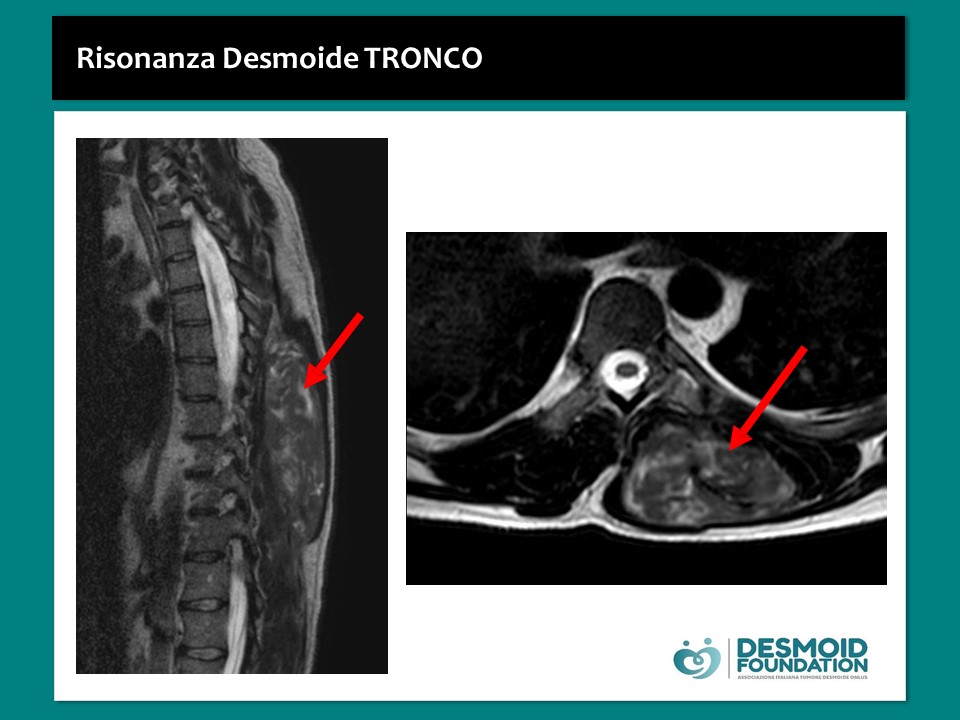
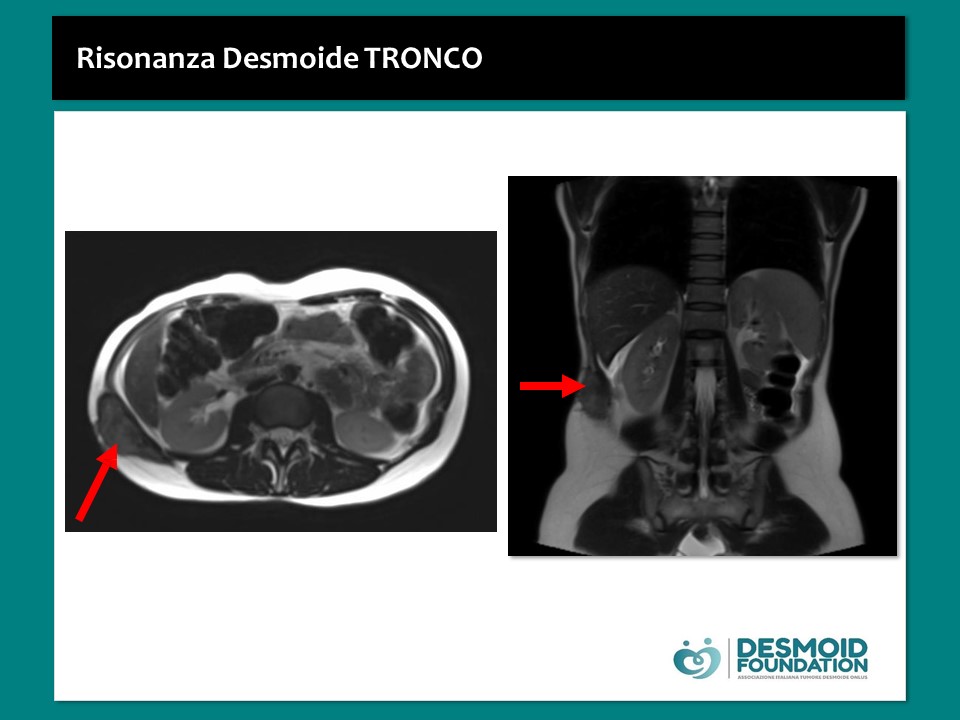
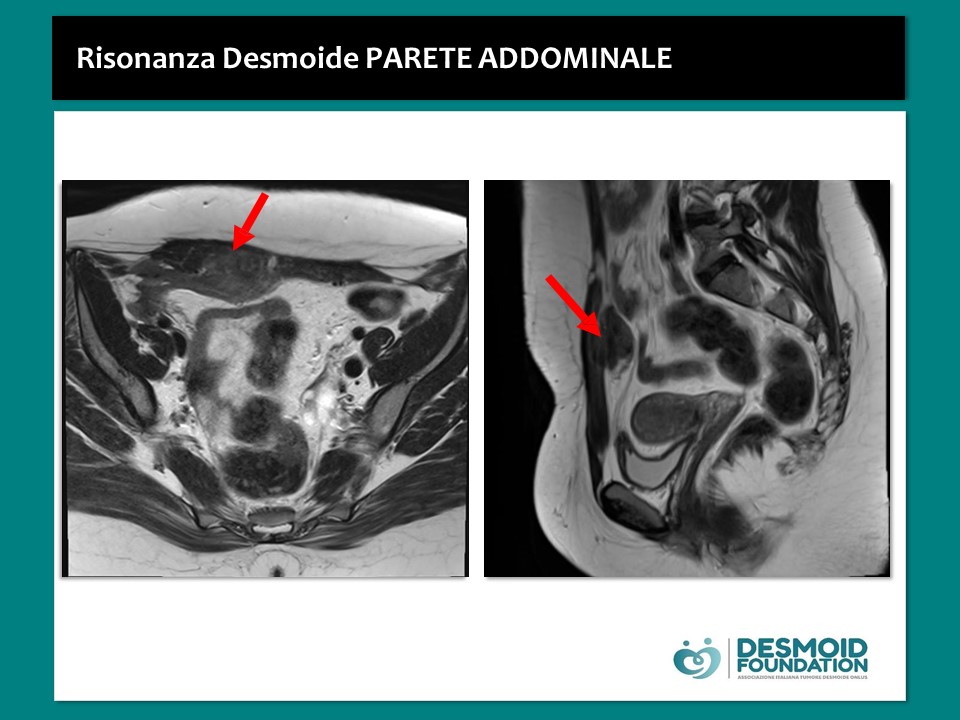
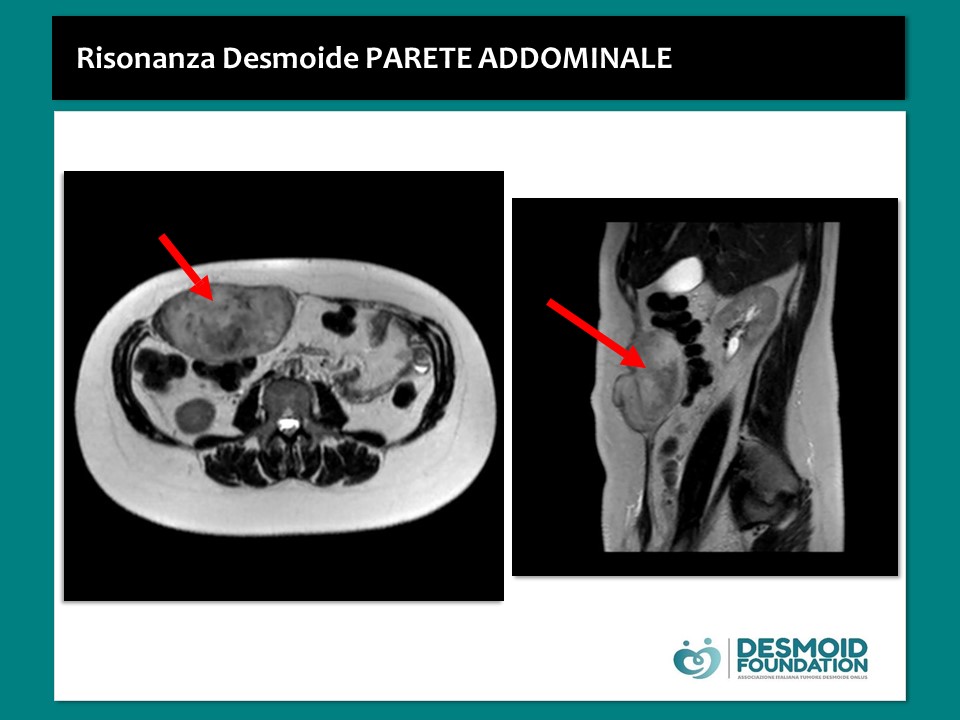
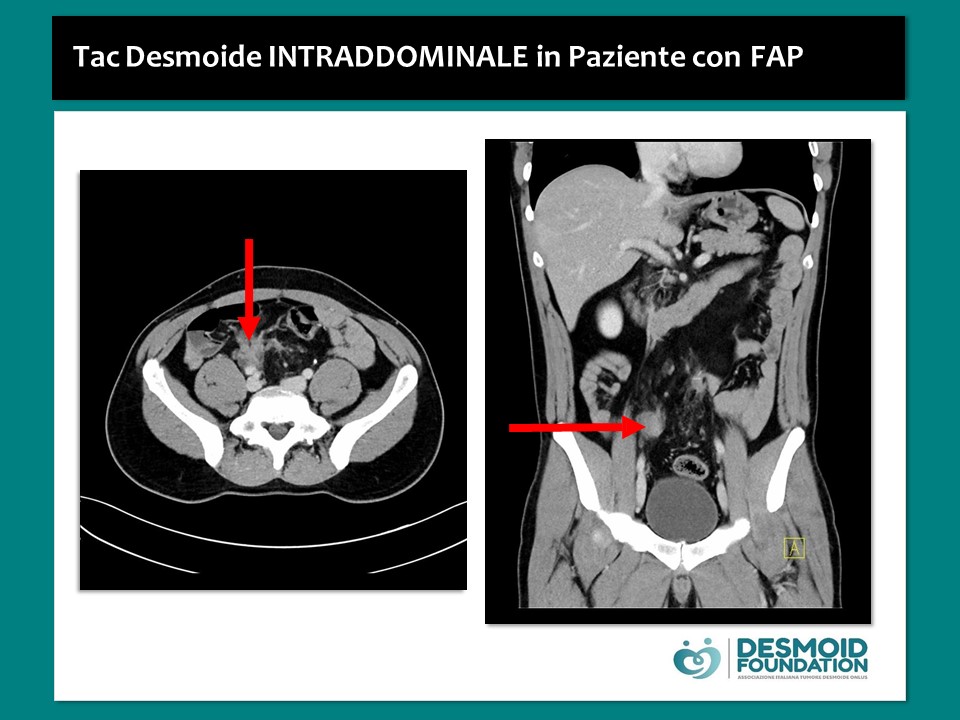
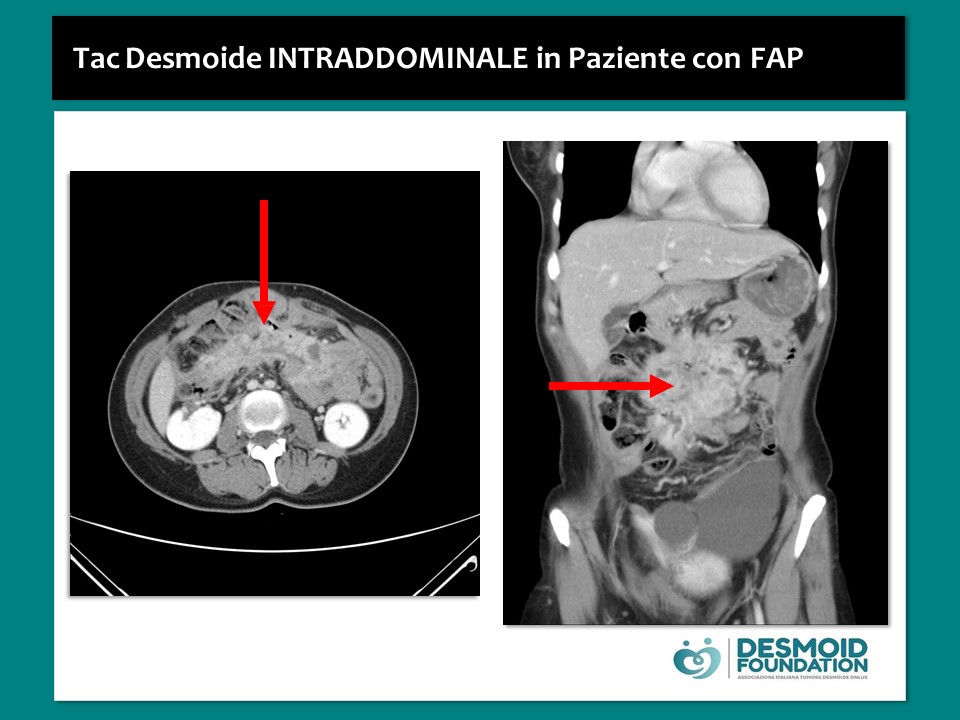
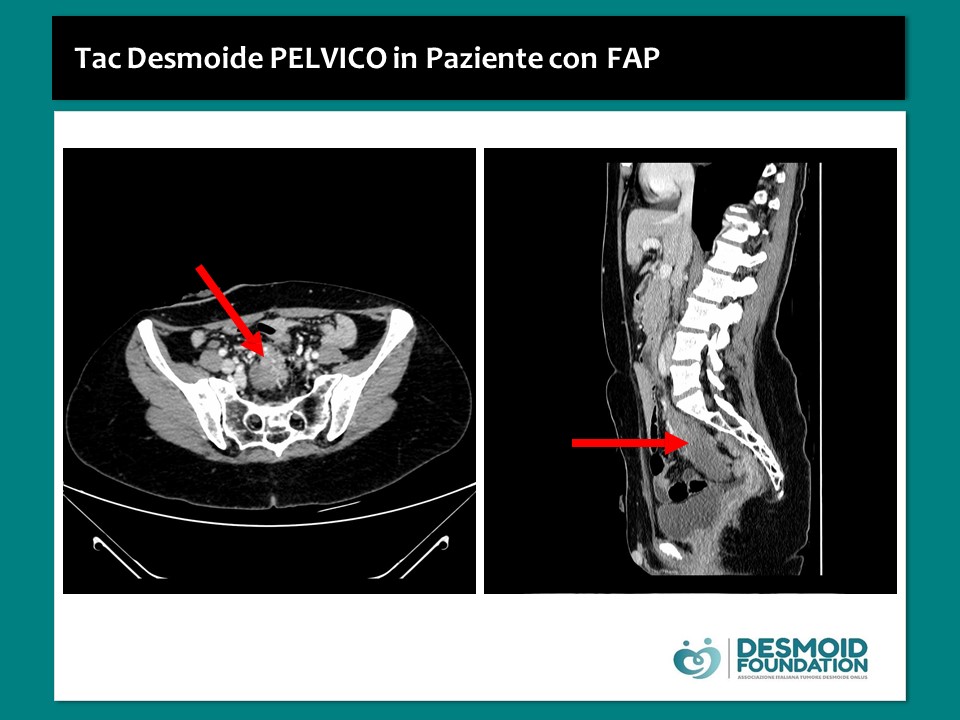
The follow-up involves the radiological evaluation of desmoid tumors of the limbs, trunk and extra abdominal sites, through the use of MRI with contrast medium; desmoid tumors in mesenteric intra-abdominal sites are better observed with CT scan with contrast medium instead.
Radiological examinations are periodically planned and the latency between one control and another depends on the stage of the disease (progression, regression or stability phase).
Generally radiological checks are planned:
- EVERY THREE MONTHS at the beginning of the follow-up, especially in the first year;
- after the checks are planned EVERY SIX MONTHS up to the fifth year;
- finally, it passes to ANNUAL checks up to the tenth year.
Controls in patients with desmoid tumor tend to continue beyond 10 years because progressions have been observed over time, albeit exceptionally.
In some cases, patients must perform an early radiological check, especially for desmoids in critical anatomical sites such as the mesenteric intra-abdominal site or the head/neck.
Spontaneous regression is observed in about 20-30% of patients and late responses to treatments are defined as those responses that occur at the end of the treatments themselves.
The evaluation of the response to treatments or of the disease itself in case of spontaneous regression or progression in patients who make the observation, passes through the use of the RECIST criteria, which are the same ones that are used for the evaluation of solid tumors and which consider only the largest diameter of the mass. They are not ideal criteria for desmoid tumors due to their particular infiltration capacity, anatomical site, morphological characteristics and possible response to treatments.
Desmoid tumor and pregnancy
Desmoid tumor is more common in young female patients during their fertile age. By studying desmoid cells, estrogen receptors are observed on cancer cells. This is one of the possible explanations why there may actually be a correlation between an hormonal state of pregnancy and fibromatosis, even if this type of correlation is not a cause-effect correlation.
There are different situations:
- Diagnosis of desmoid fibromatosis after pregnancy:
There is a considerable number of patients who have a diagnosis of desmoid tumor immediately after pregnancy or even during pregnancy. Typically these fibromatoses are in the context of the abdominal wall or near a caesarean section scar or on the rectus abdominis muscle. It is actually a very favorable localization, in fact the possibility of a spontaneous regression is higher than other ones and in case of need for treatment the success of a definitive treatment is around 90%.
- Pregnancy after a diagnosis of desmoid fibromatosis:
Many patients diagnosed with fibromatosis are into their childbearing age, so often they wish to become pregnant. During pregnancy, the speed of growth of desmoid tumors can change: doubts and fears arise in these young women; each patient should contact their oncologist if they are planning a pregnancy.
Sometimes the tumor can grow up and then spontaneously regress at the end of gestation or, if necessary, treatment can be started at the end of pregnancy. It’s important to underline that there is a very low obstetric risk for both the fetus and the mother, if you have a pregnancy during fibromatosis.
In any case, DF does not represent a contraindication to future pregnancies.
Desmoid tumor and the use of the contraceptive pill
Given the correlation between the hormonal status of pregnancy and fibromatosis, the use of the estrogen-progestogen pill as a contraceptive method is generally not recommended. However, there are not clear data of a correlation between the use of the pill and the development of a subsequent fibromatosis.
If possible, the use of other contraceptives than the estrogen-progestogen is therefore recommended. But if the pill is the only solution, this will be managed in collaboration with the trusted gynecologist.
Familial adenomatous polyposis and desmoid tumor
FAP or “Familial Adenomatous Polyposis” is a rare hereditary disease that affects 1/15,000 births, it’s transmitted as autosomal dominant (for this reason the family history is sought) and it’s characterized by the early onset of hundreds of thousands of adenomatous polyps in various segments of the large intestine.
The treatment is surgical when polyps are more than 100 because, due to this great number, it’s difficult to be able to control them endoscopically, so it is necessary to resort to surgery that involves the removal of the entire colon, or of the colon and of the rectum, in case this is also affected. If FAP is not correctly treated, there is next to 100% probability of developing colorectal cancer, usually around 30/40 years of age.
FAP is a multisystem disease and, in addition to polyposis, it can involve other extra-intestinal manifestations, and in this case it’s called “GARDNER’S SYNDROME”: the main features are osteomas (especially of the skull and jaw), dental anomalies, congenital hypertrophy of the retinal pigment epithelium and desmoid tumors. Patients affected by Familial Polyposis have an 850 times greater risk of developing desmoid tumors than the normal population, often after surgery to remove intestinal tracts due to the disease.
Recently it has been observed that patients treated with laparoscopically surgery, that is a minimally invasive technique, have a lower risk of developing desmoids, compared to a population treated with a classic open technique.
Therefore it becomes important that patients suited for a preventive surgery of colon removal, or removal of the colon and rectum, are treated with a minimal surgery because this could reduce their risk to develop desmoid tumors.
In these hereditary conditions desmoid tumors, compared to sporadic ones, have a different molecular pathogenesis due to the APC mutation.
If suspicion of FAP, to make the diagnosis it’s needed:
- FAMILY HISTORY
- Endoscopic screening: based on the identification of more than 100 colorectal adenomatous polyps;
- In the past: “congenital hypertrophy of the retinal epithelium” (sensitivity 90%) or osteomas (sensitivity 30-50%) was sought in family members, because this disease is inherited as autosomal dominant character;
- Today: laboratory research of the APC gene mutation (sensitivity 85%; specificity 100%). About 70-80% of patients have a family history of FAP, so they inherited the disease, and only 20-30% have a new gene mutation. Furthermore, it has been observed that on the APC gene, there are areas in which mutations may lead to a greater risk of being able to develop desmoid tumors. This explain why some patients need to do a more intensive surveillance.
Symptomatology: symptoms may not appear for a long time since in the early stages the disease is asymptomatic; they include: rectorrhagia, mucorrhea and blood-stained defecations.
The most frequent localization of desmoid tumors in FAP is the abdomen: in fact, 70% of patients with desmoid arising in the context of FAP have a disease with intra-abdominal localization, that can also be associated with localizations in the abdominal wall. This distribution is very different from the one observed in patients with sporadic desmoid, cause in sporadic ones other localization occur and intra-abdominal one is much rarer. The intra-abdominal localization is considered more critical because the risk of complications is greater. Furthermore, desmoid tumors in FAP are more often multifocal.
So, in relation to the more complicated localization and multifocality, in patients with FAP there is a tendency to start treatment earlier than in patients with sporadic desmoid tumors.
After a diagnosis of desmoid tumor with intra-abdominal localization, maybe with a multifocal presentation, it is correct to suspect a FAP. However, it should be considered that the probability of being diagnosed with desmoid tumor before being diagnosed with FAP is very low.
If the diagnosis of FAP is not known, the characterization of the tissue taken to make the diagnosis by mutational analysis, allows to discriminate the cases of sporadic desmoid tumor from those arising in FAP.
The medical content on this site was produced and reviewed by:
Prof. Bruno Vincenzi, Associate Professor of Medical Oncology, Department of Medical Oncology, University Campus Biomedico of Rome
Co-author Giulia Personeni, Graduating in Medicine and Surgery, University Polyclinic of Tor Vergata in Rome
With the collaboration of the IRCCS Foundation of the National Cancer Institute of Milan, Departments of Surgery of Sarcomas
SC Medical Oncology 2
The Desmoid Foundation thanks the Doctors who have kindly collaborated with the Association and that have worked to provide complete information to patients affected by this disease.
Our most heartfelt thanks to them for their commitment and time dedicated
WARNING! Informations on this site are designed to improve and to inform the patient and in general to promote greater awareness of their pathology. In no case they replace specialist medical advice. While guaranteeing the accuracy and scientific rigor of the information, DESMOID FOUNDATION declines all responsibility about informations provided on the treatments, reminding all patients to contact their specialist doctor and to evaluate with him the best treatment in a specific personal case.